Feeding Issues
Feeding issues. Every medical mom can relate to some extent to dealing with feeding issues with their child as every child undergoing health problems generally has an issue with feeding at some point. We have had struggles with both of our boys. Mason had struggles with his heart and was NG tube fed for his first month of life. Because of his heart, when he got onto bottles he needed a faster flow nipple as well as required being fed on his side. He was also on a pretty strict schedule in needing to be fed a specific volume every three hours, which had many challenges. When it came time to start feeding solid foods, Mason started out okay, until he got sick and needed to be on antibiotics. Mason ended up developing an oral aversion, and we got OT involved right away to try and help. We gave a break from solid foods until after the antibiotics and things seemed to slowly get better until there were no longer any issues, and you would never know today that he had any issues with feeding!
When it came to Dylan, one of the biggest decisions we made was a g-tube placement. He was 3 weeks old at the time and was taking all of his feeds by bottle totally fine once stabilized in the NICU. His nephrology team had a big discussion with us that it would be quickest to get a g-tube placement now, while Dylan was an inpatient, rather than when he’s discharged and having issues feeding. They also explained that pretty much all CKD kids end up being tube fed as a result of the disease. It was a tough decision to make, and with the fear of repeating the struggles we had with Mason, we decided to trust the nephrology team knew what they were talking about, and I can honestly say that was one of the best decisions we made. It wasn’t too long after we were discharged that Dylan got sick with RSV, his kidney function declined more and he stopped feeding orally. We were very thankful at this time for having the g-tube to still be able to get Dylan the nutrition and fluids that he needed.
Dylan has been ready to start solid foods for a while now with his age, and this has been another big struggle. We have had a lot of support from our renal dietitians at Children’s Hospital and thankfully one of them, Meredith, has volunteered to help answer questions that we had and that I thought other medical moms might find useful!
Here is my interview with Meredith:
Starting solid foods can be quite intimidating, especially when your child is exclusively tube fed. What advice do you have for parents who are just starting that transition into solid foods with their CKD child?
Starting solids for a child with CKD should be approached as you would for a child without CKD. The goal with initially starting solids is not volume or intake. It is learning important oral motor skills and engaging in a social experience with the people they love. Meal time should be fun and very messy! It is a time for babies to explore. Starting solids also serves a very important physiological function as it develops the oral motor steps to eating.
You do not have to delay starting solids just because your child has a g-tube or has CKD. Your baby should be ready to start solids around 6 months of age. Signs that your baby is ready include:
Hold their head up
Sit-up and lean forward
Watch for, open their mouth and close their mouth around a spoon
Let you know if they are full. For example, turns head away
Start by giving your baby small amounts of soft or puree food and gradually increase based on their appetit.
Sit down with your baby to eat. You can exaggerate eating gestures, your baby will imitate.
Let your baby explore with their hand, give them a small bowl with some food and their own spoon - it will be messy!
You can offer solid food before or after a breast/bottle or g-tube feed. Your baby will decide what works best.
What is a good starting place when first transitioning? Should you start with rice cereal like you normally would?
There really is no starting food anymore. You can start with cereal, fruit, vegetables or meat/meat alternatives! Most parents choose to start with rice cereal and progress through the grains before adding vegetables and then fruit. Really the choice is up to you. It is recommended to introduce one new food at a time and offer for 2-3 days before introducing another new food to check for any allergies or an adverse reaction. If you have a strong family history of food allergies, early introduction of these foods may prevent a food allergy from developing.
In terms of managing CKD, until your baby is consistently eating ½ cup of solid food you don’t have to worry about what you are offering. If your baby has high potassium levels in their bloodwork you may need to avoid high potassium soft foods such as bananas, avocados and mangos.
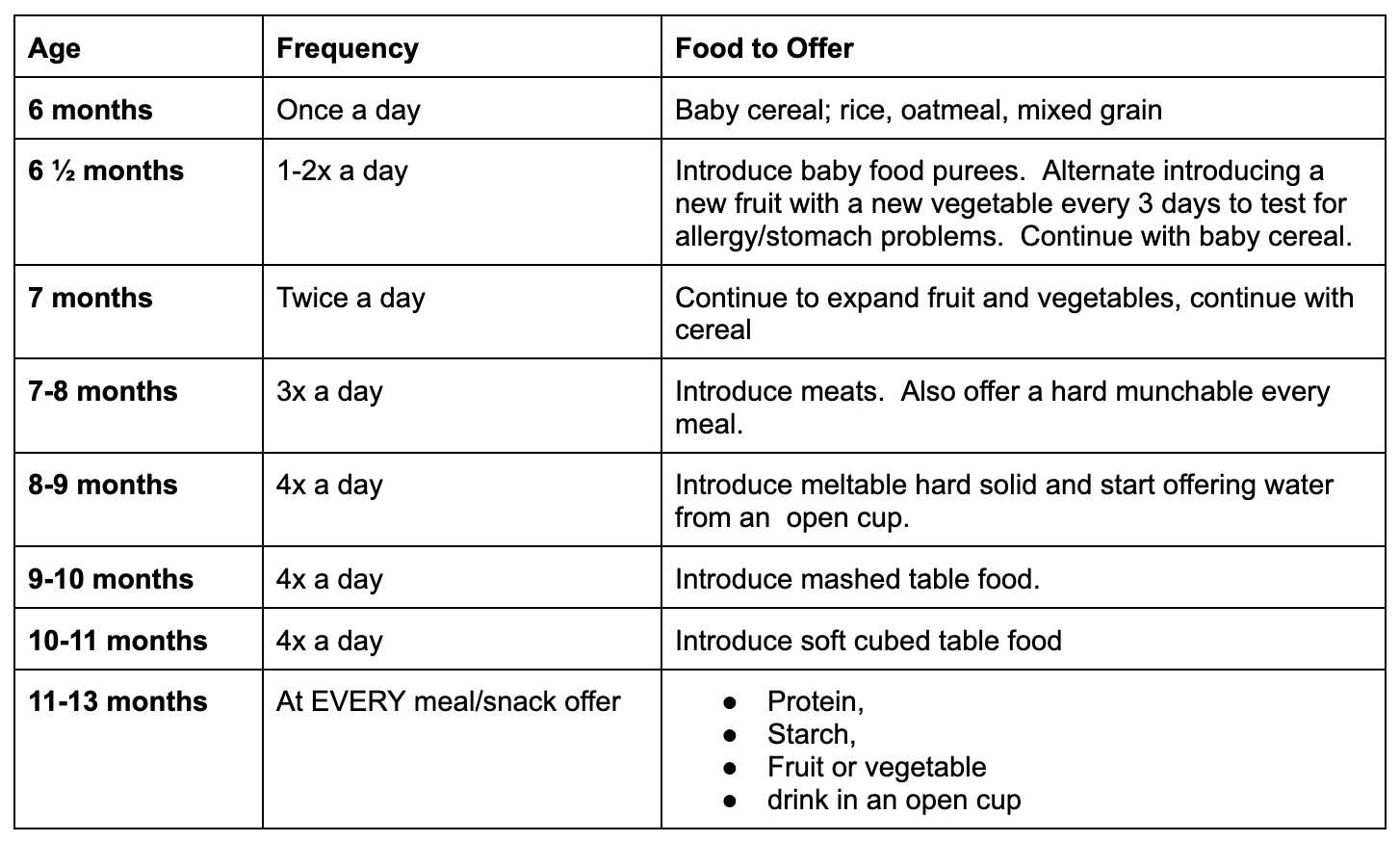
When introducing solids your baby can eat many of the same foods enjoyed by the rest of the family. The following is a general guideline for introducing solids, however, it is important to do what works best for you and your baby:
There are so many purees out on the market. For CKD children, what elements do you need to watch for on the purees? Are there certain foods or ingredients that should be avoided?
With any baby food you want to avoid any food additives such as salt and sugar. You also want to avoid any phosphorus or potassium food additives. Be sure to look at the ingredient lists of the foods you are choosing. Make sure the food you are wanting to give is the first word on the ingredients list. For example, if you are choosing a jar of sweet potatoes, make sure “sweet potatoes” are the first (and preferably one of the only) ingredients on the list. It is better to use single foods rather than mixed food items. With mixed food items all flavours blend together and there is no distinct taste. You want your baby to be exposed to a wide variety of flavours and foods as this may help them be more accepting of new foods in the long term. Avoid sugary drinks including 100% fruit juice.
Are there certain soft solid foods that are better to try and start with? Assuming banana is a bad one with the potassium in it!
Until your baby is consistently taking ½ cup of solid food we don’t have to worry about potassium in the diet. It is always good to start to familiarize yourself with food that are higher in potassium. Many baby foods do list potassium information on the nutrition label. For those that do, you can use these numbers to help you choose lower potassium infant foods:
Less than 150 mg per 120 ml (½ cup) serving = low potassium
More than 150 mg per 120 ml (½ cup) serving = high potassium
This chart gives examples of low and high potassium baby food. Feed no more than ONE high potassium food every day unless you are told otherwise. If your child has high levels of potassium on their bloodwork your dietitian will provide further education and recommendations.
When it comes to a child with CKD, is there a preference as to whether to start with purees or if you do a “baby led weaning” style?
No, please do what you feel you and your baby are ready for. You want to introduce solids as you would with any other baby. At around 6 months of age most babies can start to eat solid foods. By this time your baby needs more nutrients, especially iron. Your baby is also ready to learn about eating foods with different textures. If your child is fed by g-tube it is still very important to follow the progression of introducing solids to help develop oral motor skills and avoid developing oral aversion.
We have gone back and forth with Dylan, where we go weeks of him eating solid foods and that slowly increasing, to no solid foods at all, which is usually in relation to how he’s feeling as he wont eat orally if he isn’t feeling well. Is this typical for CKD children to have so much back and forth? It can become very discouraging at times.
Yes, there are many factors that can impact appetite and oral acceptance of solid foods in children with CKD. It is normal to have “on/off” periods with oral eating. The important thing is that you continue to offer solids, have patience, and NEVER force feed your child oral solids. If your child is flat out refusing oral feeding you can syringe purees or baby cereal through the g-tube. This will help to provide flavours refluxing up into the mouth and help to expose your baby to different flavours. You can also try the mesh food bag so that your baby can suck on food as opposed to having to manipulate them orally. Don’t be surprised if your baby is keen to put food in their mouth but will spit it out as soon as it hits the back of their throat. They may even wretch, gag or vomit. It is important that you keep this reaction positive and that you continue to exposure your child to solids in a positive way as your child needs to develop oral motor skills so they can become a skilled oral eater.
You keep answering with reference to “baby”. Dylan technically is no longer a baby, but with the back and forth of how he’s doing, I feel like we hit the restart button on solid foods and start back from the beginning. Does this all still apply, regardless of age?
His path to oral eating may take longer and he may get “stuck” at different stages in the oral motor development continuum for a longer period of time before he can move forward. It is important to pay attention to his cues and to meet him where he is at. If he has trouble handling an increase in textures he may need to go back to the beginning and take thin purees for a while then resume building on his oral motor skills with increased textures. The important thing is to not give up!
Even though Dylan doesn’t eat much at all orally, one thing that has been very important to us is making sure that he develops the skills to be able to eat orally. Sometimes this can feel like we aren’t accomplishing anything. Do you have any tips to help encourage development of these skills and continue with oral stimulation?
In order to develop oral motor skills you want to progress the texture and consistency of foods offered;
Start with thin consistency pureed foods/cereals (~6 months)
Gradually increase to thicker consistency pureed foods (~7 months)
Introduce soft mashed table foods (~7-8 months)
Introduce Hard Munchables (~7-8 months)
Hard munchables are hard food items approximately the size of a thick chunky marker. The goal with hard munchables is oral exploration only; NOT consumption. It should be something that will not break apart easily. For example; celery sticks, carrot sticks, teething biscuits, stale licorice or frozen melon sticks.
Meltable Hard Solids (~8-9 months)
Meltable hard solids are food that dissolve with spit only and require minimal pressure. Examples include; crackers, baby cereal puffs, baby cookies, snap pea crisps, cheerios, Fruit Loops and Baby Mum Mums.
Soft Cubes (~9-10 months)
Soft cubes turn into a puree with up and down pressure. Overcooked vegetables and soft cheese cubes are examples. (Avocado and banana are soft cubes but may have to be limited if potassium levels are elevated).
Soft Mechanical - Single Texture (~10-11 months)
Soft mechanical are foods that break apart in the mouth very easily such as plain muffins, soft pasta, scrambled eggs, hard boiled eggs and soft cooked beans.
Introduce mixed textures (soft mechanical table food) (~11-15 months)
Examples include; macaroni and cheese, soft chicken nuggets, spaghetti and sauce, lasagna, pizza, grilled cheese sandwich or whatever the family is having with some modification.
Hard mechanicals (~15-18 months)
Foods that shatter in the mouth and do not rapidly melt such as very crunchy crackers, hard cookies, hard raw fruit and peels, hard raw vegetables, chicken breast and steak.
At first your baby may spit the food out, that is okay, keep trying. Have patience and work on feeding skills at least once per day. If your child has a g-tube you can start putting some baby cereal or pureed food through the g-tube, this will help expose your child to taste as the flavour will regurgitate up into the mouth. It is important to continue to provide oral stimulation so your baby can continue to develop their oral motor skills.
Dylan has a very sensitive gag reflex. Often times he will put something in his mouth and if it makes him gag, then he is done oral feeding, which I can understand he is afraid. How can I help him get over this and relax his gag reflex?
Young infants have a very large gag reflex that covers almost the entire surface of their tongue. This is to ensure that if anything other than breast milk or formula get in their mouth they can get it out and won’t choke. When infants are nipple or bottle feeding, the fluid is squirted directly into the back of their throat so there is also no stimulation of their tongue. Starting solids helps to desensitize the gag reflex and move it further back in their mouth to the base of the tongue. Starting solids also helps to expose the taste buds to a wide variety of different flavours, some they will like better than others. Spitting out is okay. You may need to have a “spit” container that you hold under his mouth that he can deposit the food into. It is important that your reaction to this is neutral, neither positive nor negative. Introducing hard munchables, hard food items approximately the size of a thick chunky marker, is important to desensitize the gag reflex. Remember, the goal with hard munchables is oral exploration only; NOT consumption. It is an important part of food exploration that children feel safe that can expel something from their mouth if it doesn’t feel right.
We have involved an Occupational Therapist (OT) to help with oral feeding with Dylan. One of the biggest things we learned from OT was to have meal times (and snack time) together so Dylan can see us eating, smell the food, and have his own food if he wants. We have planned his daytime feeds around this so we are all sitting at the table together. We have Dylan with a bib, a bowl and a spoon every time. We will either have water in the bowl, a small amount of puree, or give carrots or apple slices or something we are eating to help involve him in oral feeding with us. He is always getting a feed during this time as well. Is there anything else you would recommend that could help?
I am so glad you are doing this. This is very important. Many families feed their baby separately, all by themselves. Babies and toddlers learn to eat by example. Making over exaggerated eating movements and sounds can help your baby learn to eat. Take a bite of food and chew with your mouth open making large exaggerated chewing movements, pairing this with positive sounds such as “yum, yum, yum” can also help. This sounds silly but it really does work. Children will mimic and mirror the actions they see happening around them.
One thing that is always on my mind, especially for after transplant, is that Dylan has no hunger cues. He’s always been g-tube fed and on a schedule and specific calorie intake. I imagine this is going to be a challenge post-transplant. Do CKD children eventually learn what hunger feels like? Or how much they can eat to be full? Or are hunger cues always going to be an issue?
Everyone’s journey is different and unique but to generalize, most children with end stage renal failure completely change their eating behaviors post transplant. Dylan may still need g-tube support in the immediate post transplant period, especially as the daily fluid requirement is so high. He will be able to transition to a regular nutrition supplement from the renal specific supplement and over time he may even be able to wean off nutrition supplements and use the g-tube tube for water only. The medications used post transplant also have an impact on appetite and most children have an increase in appetite and desire to eat orally.
When Dylan does start to eat more orally, how do you transition from g-tube feeds to oral feeds and still make sure he is getting the nutrition he needs?
It is important to work closely with your dietitian who will help you to slowly wean the g-tube feeds and increase oral intake while closely monitoring growth to make sure your child continues to grow along their curve and that growth does not falter.
If your child maintains an oral connection while being g-tube fed, it will be much easier to either teach them to eat or to get them to continue eating by mouth. Without this connection, it is very difficult to undo the dependence on the tube which these children can develop.
For the child who is NOT consuming ANY oral calories (ie. True swallows of food), the daytime bolus feeding should take place with the correct environmental cues AT THE SAME TIME as the oral feeding.
This is to maintain and/or make a conditioned connection between the mouth working and the feeling of getting full. We want children to understand that their mouths need to work for their tummies to get full, NOT that satiation has no connection to what they are doing. They also need to make a conditioned connection between the tummy getting full and the other environmental cues (such as the table, kitchen etc.) associated with eating. This conditioned response to the environmental cues will help the child engage in the eating process out of a built habit versus relying solely on hunger to motivate eating.
Your child will slowly be weaned off the g-tube by gradually increasing oral food consumed and slowly decreasing the night feed, while closely monitoring growth until your child is weaned.
We tend to have a lot of appointments that we go to and are always “on the go”. This can be challenging to continue with the oral stimulation, when Dylan doesn’t really eat orally, and we aren’t home. Is there anything you would recommend that we could keep in our diaper bag to always have that could help continue with oral stimulation while we are out?
While my preference is to use homemade purees or table food to feed your child as these provide the best flavour and texture exposures, “on the go” is the perfect time to use pouches, fed by spoon or jarred baby foods. Depending on where your baby is on the oral feeding continuum, I would always keep a puree, hard munchable (carrot stick, celery stick, teething biscuit, rusks or teething sticks), soft or meltable hard solids (crackers, baby cereal puffs, baby cookies, snap pea crisps, cheerios, Fruit Loops and Baby Mum Mums), soft cubes (Gerber Pick-Ups), soft mechanical (plain muffins, canned beans, diced fruit cups) in your diaper bag and ready to go.
Sometimes it can be challenging going out, and having to explain that Dylan is g-tube fed or explain why he can’t eat orally. Do you have any advice on how to talk to people to explain it?
Obviously everyone will have a different comfort level on what they want to share. I believe that people's questions come from a place of curiosity and wanting to understand. I would be honest and tell them that Dylan struggles with oral eating and he needs help to provide his body with all the nutrition it needs to grow strong and be healthy. I think the more openly we discuss this and the more we are able to educate others the less stigmatization there is around medical based interventions such as dialysis and feeding tubes. That is why I am so proud of you for starting your blog and starting the very important discussions that should occur around what it is like to parent a child that has a complex chronic disease. Too many people struggle on their own when they don’t have to. There is a supportive, loving community out there ready to help you just need to be open to making the connections and finding the resources.
I really hope this helped to answer your questions and hope that others will find this useful. Your registered dietitian is the best source of information when it comes to feeding your child with complex medical issues.